Implement the Network Contract DES: CVD Prevention and Diagnosis guidance, improve cardiovascular outcomes for your patients
Webinar:
To best use this page, we would suggest that you watch our introductory webinar. This gives you:
The content on the rest of the page will make much more sense if you watch this webinar first.
Introduction
The Network Contract DES Specification aims to reduce the impact of cardiovascular risk factors – the ABCs of CVD (Atrial fibrillation, high Blood pressure/hypertension and Cholesterol) – and to improve awareness and identification of heart failure.
The practical components of this are:
- Hypertension
- Part a
- Part b
- Atrial Fibrillation
- Familial Hypercholesterolaemia
- Cholesterol (QRISK)
- Quality improvement
- Heart Failure
Hypertension
Part A – Aims:
Improve diagnosis of patients with hypertension, in line with NICE guidance NG136, by ensuring appropriate follow-up activity is undertaken to confirm or exclude a hypertension diagnosis where a blood pressure of ≥140/90mmHg in a GP practice, or ≥135/85 in a community setting, is recorded.
This will include proactive review of historic patient records, to identify patients who have had a previous elevated blood pressure reading but have not had an appropriate diagnostic follow up.
Users can utilise the searches/reports created to identify patients who need following up and likely have a diagnosis of hypertension. We suggest users run the resources and look at the numbers of patients identified before making plans about how to approach the project. Sharing these initial findings with the PCN CVD clinical lead may be helpful to monitor outcomes.
Part B – Aims:
Undertake activity to improve coverage of blood pressure checks, by:
- Increasing opportunistic blood pressure testing where patients do not have a recently recorded reading
- Undertaking blood pressure testing at suitable outreach venues, agreeing the approach with local partners and targeting need as informed by local data on health inequalities and potentially at-risk groups
- Working pro-actively with community pharmacies to improve access to blood pressure checks, in line with the Community Pharmacy Blood Pressure Check1 Service.
Atrial Fibrillation
Aims:
Improve the identification of those at risk of atrial fibrillation, in line with NICE guideline NG196, through opportunistic pulse checks alongside blood pressure checks undertaken in a clinical setting.
Use NICE guidance NG196 to guide the identification of people at risk of AF: 3 elements to this
Aim 1
PCNs are advised to ensure that all patients over the age of 65 under-going blood pressure checks have their heart rate and rhythm recorded.
Aim 2
Where an irregular heart rhythm is identified, a 12 lead ECG is expected to be used to confirm or exclude AF:
Aim 3
PCNs are expected work with external partners to ensure that, where BP checks are undertaken outside the GP practice, the heart rate and rhythm is also recorded and communicated to the GP practice alongside the BP reading.
Familial hypercholesterolaemia
Aims:
Identify patients at high risk of Familial Hypercholesterolaemia, and make referrals for further assessment where clinically indicated.
This should include systematic searches of primary care records to identify those aged 30+ with Chol > 9mmol/L or with Chol > 7.5mmol/L aged less than 30
Subscriber resources
Simple searches/reports in all platforms to identify patients.
TPP SystmOne:
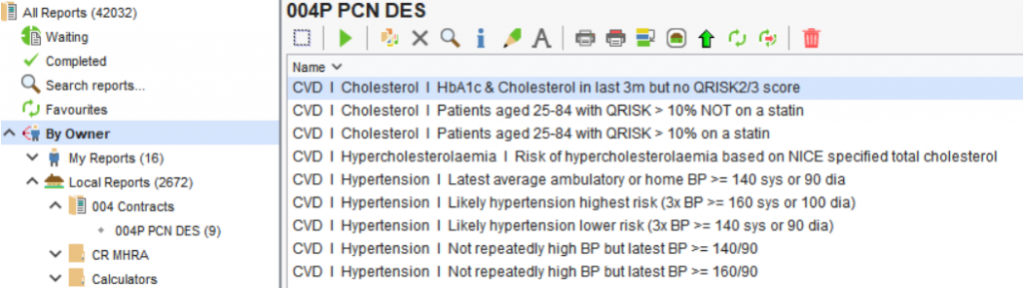
EMIS Web:

Cholesterol
Aims:
Offer statin treatment to patients with a QRISK2&3 score >= 10%, where clinically appropriate, and in line with NICE guideline CG181
Use NICE guidance CG181 for the identification and treatment of people at risk of CVD.
Aim 1:
PCNs are expected to work with the local authority to ensure uptake and delivery of the NHS Health Check is optimised for their population
Aim 2:
PCNs must ensure QRisk scores are coded for people aged 40-74years, and where possible, 75-84 years.
Aim 3:
PCNs must ensure that patients with a QRisk score ≥ 10% are identified, and that statins are offered using a shared decision-making approach in line with the NICE endorsed NHSE National Lipid Management Guidance
Aim 4:
Statin intolerance is expected to be addressed in line with the NICE endorsed NHSE National Lipid Management Guidance
Aim 5:
NICE Guideline 181 was updated in 2023 and its guidance should be followed.
Quality Improvement
Aims:
Undertake network development and quality improvement activity to support CVD prevention including:
- Reviewing outputs from CVD intelligence tools (including CVDPREVENT, when available) and sharing key learning amongst PCN staff
- Supporting the development of system pathways for people at risk of CVD through liaison with wider system partners
- Collaboration with commissioners to improve levels of diagnostic capacity for ‘ABC’ testing, including availability of ambulatory blood pressure monitors (ABPMs) and electrocardiogram (ECG) monitors
- Ensuring processes are in place to support the exchange of information with community pharmacies, including a process for accepting and documenting referrals between pharmacies and GP practices for the Community Pharmacy Blood Pressure Check Service
Heart Failure
Aims:
Additionally, a PCN must support the earlier identification of heart failure (HF), through building awareness among PCN staff around the appropriate HF diagnostic pathway, and early identification processes for HF including the timely use of N-terminal pro B-type natriuretic peptide (NTProBNP) testing
For those who have confirmed heart failure they should be additionally coded according to accepted classification (following the results of an echocardiogram). Knowing these classifications are important precursors to defining the appropriate evidence-based treatment.
These include:
- HF with reduced ejection fraction (HFrEF): Code as HFREF: 70327200;
- HF with mildly reduced ejection fraction: Code as HFmrEF:788950000;
- HF with preserved ejection fraction Code as HFPEF: 446221000
